IgG4-related disease treatment
Last updated May 23, 2025, by Lindsey Shapiro, PhD

There is currently no cure for immunoglobulin G4-related disease (IgG4-RD), but a range of treatment options, including medications and surgical procedures, are available for managing IgG4-RD symptoms and preventing irreversible organ damage.
While researchers are still trying to identify the exact IgG4-RD causes, which may help develop better treatments, abnormal immune responses are thought to drive the disease.
In IgG4-RD, certain immune cells, including those producing the IgG4 antibody, densely infiltrate tissues and cause inflammation and scarring (fibrosis). Swelling and tumor-like masses can form in virtually any tissue and organ, most commonly the pancreas, tissues surrounding the eyes, salivary glands, and the retroperitoneum, the area in the back of the abdomen where the kidneys and other organs are located. Over time, these abnormalities can lead to substantial harm to organs.
Lifelong immunosuppressive therapy may be required to keep the disease under control and prevent the onset of more serious complications that could impact IgG4-RD life expectancy.
Treatment goals
IgG4-RD symptoms often occur in a relapsing-remitting pattern, meaning there are periods of worsening disease activity — known as relapses or flares — interspersed with periods where symptoms ease or stabilize, called remission. With repeated relapses over time, permanent organ harm can occur.
IgG4-RD treatment mainly seeks to induce and sustain remission to prevent relapses and irreversible organ damage. Most people with IgG4-RD need to be treated, including those with active, symptomatic disease and those without symptoms, but with vital organ involvement.
Given that IgG4-RD manifestations can vary greatly from person to person, healthcare teams will work with patients to develop an IgG4-RD treatment plan that best addresses their own particular needs after an IgG4-RD diagnosis. Monitoring IgG4-RD treatment responses is important, as the specific plan may change over time depending on how a person’s disease activity changes, if new tissues or organs become involved, and what side effects arise.
Glucocorticoids
IgG4-related disease management guidelines recommend that first-line treatment should involve glucocorticoids. These powerful anti-inflammatory medications that derive from steroid hormones are used to suppress the abnormal immune activity thought to drive organ damage in IgG4-RD.
They’re usually taken orally, with common glucocorticoids including prednisone and prednisolone, but may be infused directly into the bloodstream in more severe cases. The exact dosing and protocol varies, but glucocorticoid induction treatment usually involves:
- higher doses of glucocorticoids to quickly induce disease remission that usually last for around two to four weeks
- patients typically entering the tapering phase, where the glucocorticoid dose is slowly reduced for some months, once the disease starts to be controlled.
Low-dose glucocorticoid maintenance therapy may be considered for patients at higher risk of relapse.
Nearly all patients see rapid and substantial symptom reductions once glucocorticoids are started. This is considered such a typical IgG4-RD response that if a person doesn’t see this improvement, their healthcare providers might reconsider their diagnosis.
The ideal goal for IgG4-RD treatment is to wean off glucocorticoids entirely, because long-term use can cause many potentially serious side effects such as weight gain, mood changes, sleep issues, bone problems, and high blood pressure or blood sugar.
However, relapse in IgG4-related disease is common during glucocorticoid tapering or after their discontinuation. As such, other immunosuppressive medications are often used in combination with glucocorticoids as steroid-sparing agents.
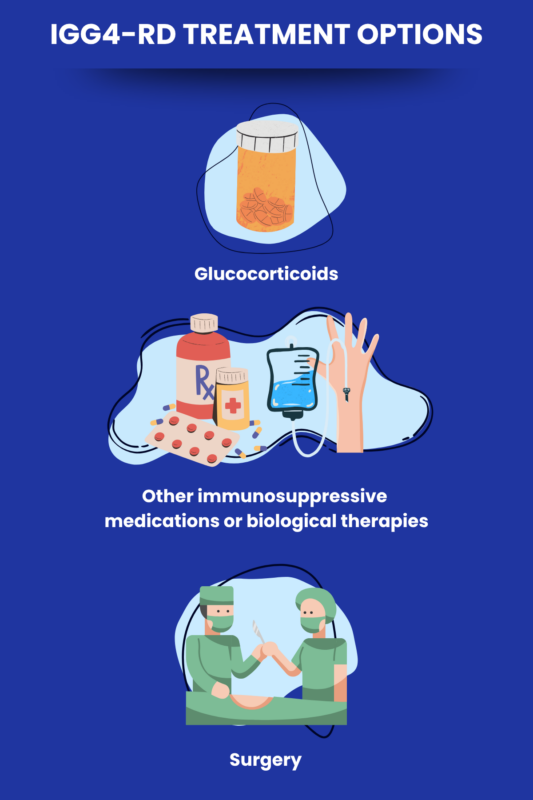
Steroid-sparing agents
In some cases, other immunosuppressive treatments may be considered in IgG4-RD to reduce the need for IgG4-RD steroids, such as:
- people with severe disease who are at a high risk of relapse or who have already relapsed with glucocorticoid treatment alone
- those experiencing severe side effects from long-term glucocorticoids.
Steroid-sparing agents that may be considered in IgG4-RD treatment include:
- azathioprine
- mycophenolate mofetil
- methotrexate
- leflunomide
- cyclophosphamide.
As with glucocorticoids, these immunosuppressants can also cause side effects, including low blood cell counts and an increased risk of infections. Routine blood work and monitoring is therefore necessary for people on these therapies.
Biological therapies
Biological therapies — those derived from living organisms — designed to more precisely control abnormal immune activity can also be used as steroid-sparing agents in IgG4-RD.
One such treatment is Uplizna (inebilizumab-cdon), the only therapy specifically approved for IgG4-RD in the U.S. Infused into the bloodstream, Uplizna is an antibody therapy that works to reduce levels of immune B-cells, including the IgG4-producing plasma cells implicated in IgG4-RD.
Another B-cell depleting therapy, called rituximab, is not approved in the U.S. for IgG4-RD, but is commonly used off-label to induce or maintain remission, even without glucocorticoids. Sold under the brand names Rituxan and MabThera, and with biosimilars available, the therapy can be used in people at a higher risk of relapse, those not responding to glucocorticoids or having severe side effects, and those not tolerating other steroid-sparing agents.
A variety of other therapies, including ones that target specific immune cell populations and inflammatory signaling molecules or pathways are actively being investigated as possible IgG4-RD treatments.
Organ-specific treatment approaches
IgG4-RD steroids and/or other immunosuppressive treatments are used regardless of which organs are affected by IgG4-RD, and this is typically sufficient to reduce disease activity and keep organ damage at bay.
However, organ-specific treatment, including surgery, might be necessary when the response to medical management is not complete or there is an urgent need for intervention.
Autoimmune pancreatitis
Type 1 autoimmune pancreatitis, characterized by pancreas inflammation due to abnormal immune attacks against the pancreas, is a common manifestation of IgG4-RD. This can cause pancreatic insufficiency, where the gland cannot produce enough digestive enzymes and insulin, a hormone that controls blood sugar. In such cases, treatment to replace missing enzymes and address nutritional deficiencies, as well as medications to control blood sugar, may be needed.
In addition, pancreas inflammation, as well as the formation of tumor-like masses in the pancreas, can put pressure on the bile ducts, the tubes that carry the digestive fluid bile out of the liver. This can stall bile flow, requiring surgical placement of a tube (stent) to keep the bile ducts open.
Sclerosing cholangitis
IgG4-RD can also cause inflammation and scarring of the bile ducts, a condition called sclerosing cholangitis. This may also narrow the bile ducts and impair bile flow, where biliary stent placement may be needed to restore it.
Retroperitoneal fibrosis
People with IgG4-RD can develop retroperitoneal fibrosis, or scarring in the back region of the abdominal cavity where the kidneys, the aorta (the body’s largest blood vessel), and other tissues are located.
This fibrosis can compress the ureters, or the tubes that carry urine from the kidneys to the bladder. Surgical intervention to enable urine flow and protect the kidneys from damage may be required, such as:
- placement of stents in the ureter
- placement of nephrostomy tubes, which drain urine from the kidneys into a bag outside the body
- surgery to free the ureters in severe cases where other treatments fail to ease the obstruction.
Retroperitoneal fibrosis can also cause aortic aneurysms, or balloon-like bulges in the aorta, that may require surgical treatment.
Orbital and salivary gland disease
IgG4-RD can affect tissues within the orbits, or eye sockets, and the glands that produce saliva and tears. In some cases, surgery to reduce bulky tissue around the eyes or remove enlarged salivary glands may help ease symptoms.
These are the interventions used for the most common manifestations of IgG4-RD, but various other procedures may be considered when other organs are involved.
IgG4-related Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Neurological symptoms may be more common in IgG4-related disease
- Guest Voice: Living with IgG4-RD is the new hobby I didn’t want
- In the language of illness, words can heal, or they can hurt
- IgG4-RD patients with allergy history are more likely to relapse: Study
- Eye muscle involvement may raise relapse risk in IgG4-related eye disease