How IgG4-related disease affects the kidneys
IgG4-related kidney disease is one of the more common ways IgG4-related disease (IgG4-RD) affects the body. IgG4-RD is a complex immune disorder that can affect nearly any tissue in the body.
Up to one-quarter of people with IgG4-RD may develop kidney (renal) issues. For many people with IgG4-RD and renal involvement, the disease also affects other organ systems.
Symptoms of kidney damage in IgG4-RD can be subtle and mimic other kidney conditions, complicating the diagnosis. The condition usually responds well to standard IgG4-RD treatments and irreversible kidney damage is uncommon when therapy begins early.
How IgG4-RD affects the kidneys
In IgG4-RD, immune cells — including those that produce high amounts of IgG4 antibodies — can enter tissues and cause inflammation, scarring, and sometimes tumor-like growths. Because the disease can affect many different organs, doctors often group cases into clinical profiles based on which systems are involved.
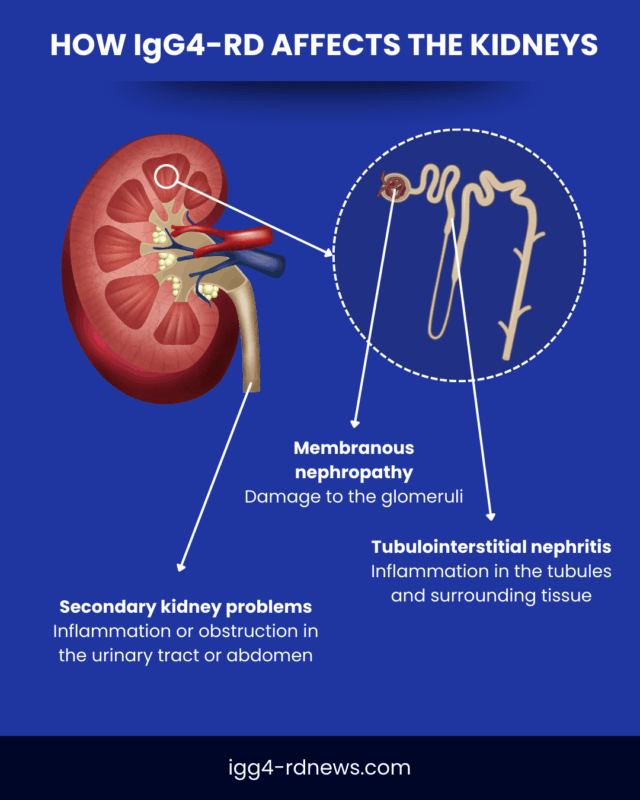
When immune infiltration occurs in the kidneys, it can lead to kidney inflammation, called nephritis, or other types of kidney disease (nephropathy). IgG4-RD can also affect nearby tissues, which may create additional, secondary effects on kidney function.
IgG4-RD-related nephropathy often develops slowly, and symptoms may not be noticeable until substantial kidney damage has occurred.
Primary kidney problems in IgG4-RD
The most common direct renal manifestations of IgG4-RD are:
- tubulointerstitial nephritis (TIN), characterized by inflammation in the tubes that drain fluids out of the kidneys, and the tissues that surround them
- membranous nephropathy (MN), in which the immune system attacks the main waste filtering structures of the kidneys, called glomeruli
IgG4-related tubulointerstitial nephritis is the most common type of IgG4-related nephropathy. It often causes no obvious symptoms or presents with non-specific symptoms of kidney failure, such as fatigue, increased urination, or appetite and weight loss.
MN is less common and often occurs together with TIN. The first noticeable symptom is usually swelling. Other possible signs include foamy urine, increased urination, or weight gain.
Both TIN and MN can occur for many reasons, but they usually show distinct features in diagnostic tests that help doctors recognize when they are linked to IgG4-RD.
Less common forms of IgG4-related kidney disease may include:
- other forms glomeruli damage
- IgA nephropathy, a condition where IgA-type antibodies build up in the kidneys
Secondary kidney problems in IgG4-RD
Other parts of IgG4-RD can also lead to kidney problems indirectly.
For example, scarring in the back of the abdominal area — a common disease manifestation called retroperitoneal fibrosis — can block the flow of urine. When urine backs up, the kidneys can swell and become damaged.
Inflammation or scarring in other parts of the urinary tract, such as the ureters, bladder, and urethra, can cause similar issues.
How IgG4-related kidney disease is diagnosed
Reaching an IgG4-related kidney disease diagnosis can be challenging because symptoms may be subtle or resemble other kidney problems. Evaluation often involves a multidisciplinary team that includes inflammatory disease specialists (rheumatologists) and kidney specialists (nephrologists).
Doctors begin by reviewing a person’s medical history to identify kidney problems or other possible IgG4-RD symptoms. They will then perform diagnostic tests, which may include:
- a kidney biopsy, to identify cellular hallmarks of IgG4-RD
- CT scans and other imaging tests, to look for enlargements, masses, or other structural changes consistent with IgG4-RD
- blood and urine tests, to assess kidney function and identify immune markers of IgG4-RD, such as high IgG4 levels
- other IgG4-RD diagnosis tests, to understand if additional organs are involved
A kidney biopsy involves collecting a small sample of renal tissue and examining it under a microscope. Kidney biopsy findings can show cellular patterns that distinguish IgG4-RD from other types of inflammatory or autoimmune kidney disease, such as ANCA-associated vasculitis, Sjögren’s disease, and sarcoidosis.
Routine kidney function tests in IgG4-RD may be recommended even for those whose disease primarily affects other organs. This helps detect and treat kidney involvement early.
What to expect over time
As with other forms of the condition, IgG4-RD treatment for kidney disease typically involves glucocorticoids (steroids), a strong type of anti-inflammatory medication. Standard steroid treatment for IgG4-related kidney disease begins with a higher dose that is slowly tapered to a lower maintenance dose or, in some cases, stopped entirely.
Most people respond well to steroids, but relapses can occur, especially if treatment is reduced or stopped too soon. In the long term, managing IgG4-related kidney disease may also include other immunosuppressant medications to help prevent relapse.
If kidney problems are secondary to obstructions caused by other IgG4-RD manifestations, surgery may be required to relieve the blockage.
Treatment works best when started early, before the kidneys are significantly damaged. Without treatment, IgG4-related kidney disease can progress to end-stage renal disease, where the kidneys are no longer able to perform their necessary functions. At that stage, dialysis or a kidney transplant is needed to replace kidney function.
People with IgG4-related kidney problems should maintain a regular follow-up schedule with their clinical team so treatment response and disease activity can be closely monitored
IgG4-RD News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by